Reducing the stress of modern mammalian motherhood
Solutions! When the stress is layered and the connections are extensive, the stress-reducing strategies need to go far beyond personal responsibility.
When it comes to breastfeeding and baby feeding decisions, the stress is layered, the connections are personal and, somehow, also universal.
So far, we’ve examined the mental health outcomes related to this stressor node:
And then dug deeper into the layers with an eye on solutions with
— support without judgment being key:Surprising (well, not at all surprising), there is still more to tackle here when it comes to tying together all the elements that relate to the stress of breastfeeding + baby feeding.
As you might expect, the links between maternal health outcomes and stress/stress perception and breastfeeding/baby feeding fall right into the research gaps. And, again, these gaps may have something to do with the way most research prioritizes baby’s health while masquerading as a maternal health focused study.
Because I just can’t help myself, an example — a review on maternal stress, breastfeeding, and cortisol with this terribly confusing statement: “It is of great importance to study how stress affects the high rates of premature relinquishment of EBF [exclusive breastfeeding]” (and if you need a reminder on why the metric of “premature relinquishment of exclusive breastfeeding” is problematic, go back to the first post.)
Besides the ridiculous language, another important consideration with this review is that ALL of the studies included in the review use cortisol as a metric for maternal stress. Which wouldn’t be terribly problematic if we had a full grasp on how cortisol is regulated during the transition from pregnancy → postpartum → lactation… but we don’t. Cortisol regulation during this life stage is complex and there are a LOT of question marks that still require lots of basic science to catch up. Plus, research has shown that the physical act of expressing milk actually decreases cortisol levels and dampens the stress response.
So, when that problematic review concludes: “EBF rates at hospital discharge were influenced by mothers' perceived stress without a direct relationship to cortisol levels”, I am not surprised by that. Cortisol, even though it is the “stress hormone”, is a bad metric for stress during this life stage.
Maybe its just the one review? Nope, here’s another one. Same problem. And another. Same prioritization of baby. Do I seem annoyed? I am. I’m absolutely exhausted.
So here we are, with something that I stated in an earlier post:
“research has not connected all the dots BUT we do know that stress (even in the form of clinical delivery, lack of support, and overall mom guilt) is bad during this window of time.”1
I fully recognize that, by its very nature, the perinatal period presents a bunch of situations that match the hallmarks of acute stressors — unpredictability, lack of control, and novelty — so some stress is absolutely unavoidable during the stage of life. However, the sources of stress that I am focusing on with this project are the (theoretically) avoidable stressors – the stressors created by and/or exacerbated by the structures and systems and societal pressures that we work within as American mothers and caregivers and birth parents.
When it comes to internalizing external, psychological stressors, perception – how the brain interprets and processes the external stimuli – plays a significant role in how the body kicks off a physical stress response. Overstimulating the stress response or failing to shut it off ultimately leads to the health effects of chronic stress.
While the research linking stress + breastfeeding / feeding decisions + health outcomes are weak for the reasons explained above, the added factor of “timing” of this stressor node plunks it squarely during a life stage that is particularly sensitive to the risk of added stress. The postpartum period is a moment of rapid change and recovery. The physiological house of cards stacked up to the top during pregnancy is being rapidly dismantled:
This means the health risks of stress are exponential but so are the long-term benefits of limiting stress (FOR THE MOTHER… and, sure, baby too). This is the time of life when those controllable, external stressors should be as limited as possible. That is not the case today (it is the exact opposite, especially in America) and that is what we can work towards changing.
So where do we go from here?
If it's the challenges of breastfeeding that causes stress, then how do we eliminate some of the challenges of breastfeeding? If it's the shame and guilt around feeding decisions that causes stress, how do we eliminate the sources of that shame and guilt? If it’s a lack of control (because true “choice” around baby feeding does not exist in the current structure of support at home, at work, in healthcare, in society) that causes stress how do we change the system and allow for personal decisions to be personal decisions?
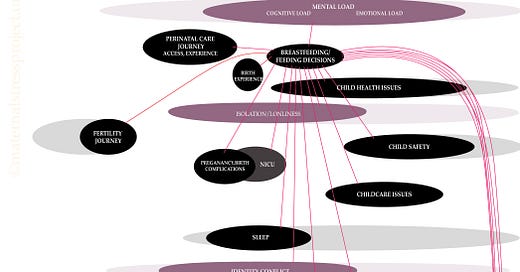
Let’s start with a cleaned up version of the stressor map, highlighting all the connection points:
The connection points represent other potential maternal stressors that could change the perception of the breastfeeding / feeding decisions stressor node (for better and worse). The connections represent risk but also opportunities for stress-reducing solutions.
Most of the connection points came up in my discussion with
:Additional connections to consider include: workplace discrimination, housing security, food security, and the societal experience of marginalized communities especially as it relates to racism.
(Quick reminder – This project is a work in progress. If at any point, I miss something or gloss over or exclude a core concept that could play a valuable role in this discussion, let me know! I’m learning as I go and you are a part of that journey.)
Some ideas on broad solutions:
Paid Leave
The American Academy of Pediatrics recommends exclusive breastfeeding for six months and then continuing for two years.
Two years.
We do not have a federal paid leave policy in America. There are moms returning to work immediately. Even a “good” leave policy averages around four months. So… to “exclusively breastfeed,” the expectation is that lactating parents pump their breast milk when they return to work. (See pumping at work + workplace support + mental load + social narrative below)
Stress can come from that conflict – the mismatch between medical recommendations on length of time to breastfeed and our nation’s failure to provide families with the opportunity to have that time without work-related constraints.
Imagine how passing a federal paid leave policy will lift the weight on all those stressor connections?
Join the fight for Paid Leave here. Or check out the cross-sectional work of Chamber of Mothers and Moms First.
Child care access
We are in the midst of a growing child care crisis. If child care centers continue to close and/or become financially out of reach, more lactating parents might keep younger children home while nursing an infant (assuming, of course, they have access to paid leave or the financial stability to make that choice). Imagine having a toddler at home while facing breastfeeding challenges? Imagine having a nursing baby in the NICU and a toddler at home. Add in the stress of finding child care for both that toddler and your infant…
Continue pushing for federal child care policy here.
Changes in medical reimbursement
Again, lactation support is key. Education can calm the feelings of lack of control and prepare for the unpredictability of challenges (both drivers of the stress response). We need coverage of comprehensive postpartum care with access to lactation support beyond Labor & Delivery. Technically, lactation support should be covered as preventive care, but, well, there are issues with that. Andrea breaks this down very well with emphasis on the importance of available lactation support services (like SimpliFed) working with Medicaid recipients.
Formula regulation + de-stigmatization
I really wish someone studied the stress load on parents during the infant formula crisis in 20222. If you lived through it, I apologize if this is triggering for you. The recalls by companies that control the market and lack of government planning/quick action caused a shortage that left shelves empty across the country and families frantic.
This plays into the stress related to child safety concerns (possibility of tainted formula), identity conflict and the social narrative (the “bad mother” feeding formula), and mental load (where to find formula in the middle of a formula crisis). Solutions here relate to federal regulation standards but there is also a need for more formula options, especially for companies that also work towards changing the narrative, like Bobbie or ByHeart. There is current legislation on the table to make this happen.
Legal protections for pumping at work
Returning to work at any point in the breastfeeding journey (see Paid Leave section) adds additional connections that play into the perception of breastfeeding and feeding decisions. It may relate to not having true “choice” in the decision, amplifying the sense of lack of control. Filter this through the stressors related to workplace discrimination, especially for those who may not be able to speak out for fear of losing wages or their job altogether. While there was a big win with the PUMP Act passing in 2022, requiring most businesses to allow break time and a private place to pump at work, it will still take time for everyone to become compliant.
Make sure your workplace is aware of what they need to do according to federal law.
Getting paid for unpaid labor
Ok, I haven’t thought this one through but it came up recently in a fascinating conversation I had with a friend in the maternal health space – what if we quantified the time spent breastfeeding + pumping and PAID lactating parents for that work? Maybe this goes into the adding unpaid labor to the GDP conversation. Either way, the goal is to change the way we value women’s time and how we value the time that lactating parents put towards feeding their little Americans.3
Some ideas on community solutions:
Workplace support
Want a glimpse inside the mental load of pumping on a work trip? Come with me to the Consumer Electronics Show in 2016. Now imagine how this load would lighten with accessible lactation space like a Mamava pod, a breastmilk shipping service like MilkStork, or more discrete and/or innovative breast pump like Babyation or Willow Pump (fun fact: Willow launched at CES the year after I wrote that and they had a laminated picture of me pumping in the bathroom!) or tools to facilitate the stress of pumping4, like Lilu.
Any way you can reduce the mental load of a pumping colleague/employee returning to work will go a long way.
Bonus points for providing resources like The Fifth Trimester or Pheobe to help guide the transition.
Culturally competent, respectful care
I am not anywhere close to an expert in these areas so I will lean heavily on those who I have spoken with up to this point and continue having those important conversations. One discussion with Dr. Kobi Ajayi (and that one will be written about soon too!) comes to mind in the context of Black mothers in the NICU: the critical importance of social support, education, and respectful care when it comes to breastfeeding. In addition, having access to resources like the Irth app can be a valuable way to ensure a care team becomes a stress buffer rather than a source of additional stress.
Social narrative —> No judgment
I’m not sure how this one plays out but it's a reminder, again, that language matters. You have no idea how a simple word filters through that stressor map for an individual and exacerbates the stress they are already experiencing. This may relate to the healthcare community (see discussion with Andrea on scripting), it may relate to discussion in mom groups, it may relate to a seemingly simple question you ask a colleague returning from maternity leave. This is especially important for parents who combo feed and formula feed.
This one is something we can all work on.
Some ideas on family / friends solutions:
Give the gift of sleep
Sleep is a circular stressor: stress affects sleep and lack of sleep = stress and then that stress affects sleep even more.
Yes, I know, I know, sleep disruption feels inevitable when the hungry human needs to eat at 1am and the food source is attached to your body.
However, as an example, consider how sleep is affected by paid leave — especially when the non-birth parent does not have access to leave and everyone operates around the assumption that “they need their sleep to work…” Current sleep priorities tend to favor the working partner even though the person who really needs to sleep is the postpartum parent. Add in difficulties and challenges with feeding and that middle-of-the-night cry may hit the brain just in the exact spot at the worst moment.
“Just telling a mother to sleep is as ridiculous as telling her to fly. Protecting her sleep requires challenging deep cultural and structural factors, both within families and within the medical establishment.” – N. Leistikow et al. 2022
I appreciate this Commentary piece in Biological Psychiatry. The authors recommend a “sleep prescription” for postpartum depression with the weight on the family and community:

A key opportunity here is to reassess who takes on what role at night. I have already expressed my thoughts on how division of labor in the home around nursing+sleep relates to wakefulness and long-term emotional labor load.
Be that helper or help find that helper.
Divide mental and physical unpaid labor load at home
The birth parent tends to take on a bulk of the mental load and unpaid labor load related to feeding that baby, especially when they are the only ones in a partnership that have paid leave after baby’s arrival.
Mental load tends to be gendered. From a stress perspective, I think of mental load as “one more thing on the pile” that all other stressors filter through in the brain; a potential source of stressor exacerbation. But that isn’t a very scientific assessment because the science has not been done yet.
Partners can help lessen the impact by taking on more of the mental labor load. Check out Eve Rodsky’s Fair Play and
’s Equal Partners for tips on where to go from here.Help find lactation support
I remember getting a “breastfeeding basket” during my baby shower – nursing bra, pads, nipple cream, breastfeeding pillow – and, honestly, it won the day (and important to note: that friend checked in with me first about my plans to breastfeed).
Even better – help a friend find or even sponsor their lactation support. For example, tell a friend about SimpliFed (insurance may cover it!) or you can send a gift card (again, I am not getting any kind of compensation from them, I just love everything that Andrea stands for and the product she has put into the world)
Oooh, that was a lot.
BUT it is not a comprehensive list and the science behind all of this is weak (should I shake my fist at gappy science again?)
I do want to point out a key thing missing here in the solutions list: personal responsibility for managing the stress.
The stress and stress-reducing solutions related to breastfeeding / feeding decisions exist outside of personal responsibility. When stress relates to structural, societal, and community support issues, the solutions need to come from structural, societal, and community support changes.
What am I missing?
On the connections side: test out yourself and chime in below.
Consider your own infant feeding journey, ask a friend or colleague. Trace personal interconnections between your perinatal care, birth experience, sleep, return to work, social narrative, isolation/loneliness, unpaid labor load, mental load, child care, etc. What am I missing? What layers within this stressor node or the connection points have you experienced? What other solutions can we see here?
Quick note about subscriptions: The Maternal Stress Project is an educational and idea-spreading initiative and I want it to be available to all. You can subscribe for free and get all posts delivered right to your inbox. However, if you feel compelled to bump up to a paid subscription, your generous support will facilitate the growth of this project… and be much appreciated!
Sharing and spreading the word is equally valuable and appreciated!
Quick caveat: whenever I make a statement implying that “stress is bad”, it relates to the elevated risk of stress-related illness during the perinatal period. Some stress is good!
You will not tempt me down the rabbit hole of the effects of “toxic stress” on baby because I feel that the language used there tends to blame and shame mothers and, well, that’s another stressor!
Maybe you did? If so, get in touch!
The other side of this is to accept that US is a hyper-capitalist society where the prevailing view is that everyone has to earn their keep. But most of parental caregiving, including breastfeeding, is not included in our GDP. It’s not just unpaid labor but it’s unseen. How would views on these social policies change if the labor and output of breastfeeding was viewed as an essential part of our nation’s economy? In this view, it’s less of a solution and more of way to generate momentum for our leaders to adopt solutions.
The stress of pumping extends beyond the workplace, of course.









It's another fantastic article, Molly. There are so many great points made that it feels like I'll need to revisit it over and over again. But one thing is certainly clear - to reduce the burden stress has on mothers, there is a need for systemic changes rather than singular, sporadic strategies (like educating women about the benefits of breastfeeding without legal provisions for pumping, maternity leave, or childcare places for older siblings).
I appreciate your point that stress-reducing/mother supporting strategies need to go beyond personal responsibility. Certainly parents need to strategize on a personal level, but so many of the obstacles and barriers we face (e.g. childcare costs) are part of a larger systemic problem. Thank you for this fantastic article, Molly.