"Breastfeeding and baby feeding are connected to all of this"
Digging into connections and solutions with Andrea Ippolito, CEO and founder of SimpliFed
From a biological perspective, breast milk is a wonder.
From a stress perspective, that statement alone can be a trigger.
How do we tease apart the stress related to breastfeeding and feeding decisions in the broader context of maternal health when it is so intertwined with societal expectations and narratives, and, far too often, lack of true “choice”?
To dig into allllll the layers of this stressor node (and solutions!), I turned to
, CEO and founder of SimpliFed. SimpliFed is a lactation support telehealth company that provides compassionate, human-to-human support and education at all stages of the breastfeeding journey.As discussed in the previous post:
We have to balance the value and importance of breast milk and breastfeeding AND accept the stress that breastfeeding exposes individual lactating parents to. We have to fight for education, lactation/feeding support, and other broad solutions to limit exposure to the stressors associated with breastfeeding/feeding decisions AND view breastfeeding/feeding decisions as a stress-inducing risk factor at an individual level.
If you missed it, read here:
As for solutions sitting squarely in this stressor node: “support without judgment is key – in healthcare, at home, in the workplace, amongst friends, in social media feeds. Language matters.”
Andrea and SimpliFed embody this.
Here we go.
MOLLY
I love that one of the first things you have on the SimpliFed website is “91% of the patients report feeling less stressed after working with us”.
Can you talk about your journey a little bit – how you became interested in maternal health space and how transitioned into focusing on breastfeeding and feeding support?
ANDREA
When I had my first daughter, I saw that there is this deep connection between feeding her and my physical and mental health. I live in Ithaca, New York, which has the highest breastfeeding rates in the state and the highest density of lactation consultants. So if I was feeling this way as an insured, privileged, white woman who's married to a physician in an area with the highest density of lactation consultants, in the county with the highest breastfeeding rates then how the fuck is everyone else doing this?
I have never felt so lost and broken, felt so unprepared for the ridiculous no-days-off, no-nights-off tasks that was breastfeeding.
If I felt this unprepared, there's got to be a better way.
“if I was feeling this way as an insured, privileged, white woman who's married to a physician in an area with the highest density of lactation consultants, in the county with the highest breastfeeding rates, then how the fuck is everyone else doing this?”
Feeding, no matter how you feed, but especially with breastfeeding, is so deeply connected to health, it is clinical and it's not recognized that way.
Fast forward, [I just had] my third kiddo and I was in so much pain. Toe curling pain, blood everywhere. Most women don't have support to work through that and then you are told to “buck up”. You end up suffering in silence, often in the middle of the night. Thankfully I had a ton of support because I had access to support that was covered by insurance. At no cost to me.
Breastfeeding is great for 1000 reasons, but seeing how deeply connected it was to my physical health, to my mental health; knowing that most families are left to toil by themselves; I just kept thinking that there's got to be a better way.
MOLLY
So, correct me if I’m wrong – the Affordable Care Act starting covering lactation support as preventive care, right?
When did that happen and what did that open up for SimpliFed and lactation support in general?
ANDREA
You bring up a really important point about the policy that not a lot of people have – it's nuanced. The National Women's Law Center does the best job of summarizing it. It's a WPSI Women Preventative Health Service recommendation, and because it's part of that, as a preventative service, that's where the mandate comes in.
Now the interesting part about how this all played out. ACA was technically implemented as part of a January 2012 CMS guideline. Now, there were a few pieces to it. There was a piece on breast pumps getting covered. And, most importantly, counseling is also covered. The pump part of it was very well implemented. Arguably, a decade ahead of the lactation support. And then there was a “wait a second – you can have lactation support and counseling as well” moment. People miss that part because they thought it already existed. It exists in Labor & Delivery. It exists as part of postpartum care, like in pediatrics. It exists as part of the Global Maternity payment.
But, it's supposed to be a separate reimbursable expense starting during pregnancy for as long as a person needs it. The problem is that it doesn't get implemented because the main people that have these contracts, health plan contracts, healthcare systems, are also accepting Global Maternity payments. The global maternity payment is extremely low - on average about $1500-$3500 per patient with Medicaid beneficiaries, so adding in an additional service like breastfeeding support is extremely difficult because there is no money left in the global.
“[lactation support and counseling are] supposed to be a separate reimbursable expense starting during pregnancy for as long as a person needs it. The problem is that it doesn't get implemented.”
According to the policy, it should be a separate reimbursable expense, but most families don’t have access to it in an ongoing way outside of Labor & Delivery. Patient support isn't part of the care pathway, because healthcare systems don't get paid for it. Long story short, you really have to get into the muck of policy to understand what's happening.
This absolutely affects why mom's mental health is suffering right now in relation to breastfeeding. You are told to “buck up” or “get support in the hospital”, but at that moment, you are recovering. Or you're barely recovering. If you had a C section or a vaginal delivery, you don't know which way is up. You’re bleeding tennis balls and blueberries and you're trying to figure out this whole breastfeeding or baby feeding thing and, by the way, your milk hasn't even come in!
Physiologically speaking, Labor & Delivery is not the best time to get support. But that is when most women have this service available to them.
MOLLY
From the research perspective on maternal mental health and breastfeeding, the connection between the two seems to go in both directions – breastfeeding improves maternal mental health or maternal mental health improves breastfeeding.
When you factor in the mother<>infant dyad, whose health are we most interested in? Usually the baby’s, right? It still feels very lopsided in terms of the research of whose health outcome are we most concerned about.
Do you feel that way too? Like the maternal health part of the equation is a stopover to get to the child health side? We’re not concerned about the mother?
ANDREA
The baby's health is definitely prioritized over the mom's health. And so that impacts care delivery and goes back to reimbursement. You are able to get those wellbaby visits reimbursed. That's the pediatric care pathway. The six week postpartum visit is covered as part of the Global Maternity Bundle and sadly it is abysmally low so nothing else is covered. You have to follow the money. The money shows you that we don't prioritize the moms health postpartum.
It is starting to change. It is 100% starting to change. But it is nowhere near where we need it to be.
“The baby's health is definitely prioritized over the mom's health. And so that impacts care delivery and goes back to reimbursement.”
Baby feeding is connected to maternal mental health. Breastfeeding advocates say: “oh, folks that are breastfeeding have lower rates of postpartum depression”, but how does the data breaks down when you consider someone that is breastfeeding and has actual support from a lactation consultant or a trained healthcare professional, versus what the postpartum depression levels are for folks that did not [have support]? And then the same thing with formula feeding and combo feeding. Most parents combo feed so it's hard to disentangle. I'd like to see how those numbers break down for those without professional support.
MOLLY
I found a literature review on this recently. I like literature reviews instead of individual studies because when you’re relying on single studies, you can find a paper to justify whatever you want. And research is not wholly unbiased – if you're going to study the positive effects of breastfeeding, there might be some self selection in the sample or you might flatten the results with averages, or you might not publish at all if you get negative data because no one likes to publish negative results. We can go into the bias of science and science reporting but I’ll get back on track.
In the nuance of it, you might see positive effects of breastfeeding on mental health, but as you point out, there could be a whole other subset that is a little more nuanced in who has support, who has challenges, who has additional unquantified issues related to identity and social pressure.
And when you layer in that nuance, you do see, in the research, how breastfeeding can negatively affect maternal mental health.
So what this review was examining was the “some go this way, some go that way” side of the overall research pool. And the differences do relate to support, they do come down to all these different elements.
If it's the challenges of breastfeeding that relate to stress and push you over the edge, then how do we eliminate some of the challenges of breastfeeding? That's what you're solving for with SimpliFed. And that's not always acknowledged or supported financially.
ANDREA
Yes, something that would be interesting to study: do you have a partner and/or family support?
We just heard from someone two weeks ago that her husband is making her breastfeed even though it's not going well for 1000 reasons. He is making her breastfeed. Not even letting her pump. And she was in so much pain. So like, how stressful is that? To be dealing with pain and also pressure from family?
Another important consideration: ability to buy all the stuff. For me, I was able to buy the my breast friend pillow, which is like 40 bucks but makes breastfeeding so much easier. I was able to buy nipple creams. I was able to buy the Willow Pump in addition to my insurance covered pump. I was able to buy the nursing pads. And, yes, some of that is covered by insurance. Most people don't think of all the extra shit that made breastfeeding a little bit easier and factor in the financial side of breastfeeding.
“We just heard from someone two weeks ago that her husband is making her breastfeed even though it's not going well for 1000 reasons. He is making her breastfeed. Not even letting her pump. And she was in so much pain. So like, how stressful is that? To be dealing with pain and also pressure from family?”
MOLLY
On that note, SimpliFed accepts Medicaid patients, is that correct? Can you speak to the importance of making sure more people have access to the services like those you provide?
ANDREA
It is the right of families under federal law to have access to breastfeeding support services and most Medicaid health plans are not in compliance with federal law in this realm. Medicaid beneficiaries account for 44% of all births in this country and they serve the highest quality care starting during pregnancy. SimpliFed designed our administrative processes from the beginning to be able to serve Medicaid beneficiaries and we waded through quite a bit of bureaucracy to get Medicaid contracts setup. After TRICARE, Medicaid contracts came next for us, then commercial contracts.
MOLLY
For additional stressors, the social narrative or connection with social narrative – what we're seeing in the world, social media, friends, marketing, and how we feel about ourselves. One of the metrics in the review I mentioned actually caught me by surprise: Maternal Role Attainment.
Do you know about this one? Maternal Role Attainment, they call it MRA for short, is a metric that researchers used as a subscale of “breastfeeding success” – it’s the interpretation of individual success. It has nothing to do with how long or how short the individual actually breastfeeds. MRA, as a metric in this context, relates to the extent to which a woman views her own standard of “successful breastfeeding” as an important part of her identity as a mother. A higher MRA score relates to a stronger attachment to this identity, the feeling that they are a “good mother” if they “succeed”.
For breastfeeding, the higher the MRA, the more likely that individual is to breastfeed. BUT for those with a higher MRA, if they stop breastfeeding “early”, then they have a higher incidence of clinical depression compared to those who stop breastfeeding and have a lower MRA.
I find this so fascinating because it really ties the potential health effects of identity and also identity that is potentially driven by the social narrative around breastfeeding. It speaks to challenges and attempts to overcome challenges and the hardship of failing or feeling like you’ve failed.
ANDREA
Yeah, it’s a lot!
Reminds me of this badass orthopedic surgeon who had to stop breastfeeding with their second kid. She was like “yeah, I had postpartum depression because of it.”
MOLLY
I always find it fascinating when we instinctively know how it's all connected. How a first reaction is “I was forced to stop breastfeeding. I didn’t want to. And that led to my postpartum depression.” Anecdotally, we know, but the research is still so gappy.
What would be your: “if only XYZ research existed, it would really help make this picture more full”?
ANDREA
I think the level of family and partner support. Access to other financial resources. Studying combo feeding and not treating studies like a monolith of breastfeeding versus formula. I think most people do both. It's not just one or zero for most people.
I would be really interested to see emotional and mental health outcomes for combo feeding compared to those who are totally breastfeeding or totally fully formula feeding. My hypothesis is that the halfsies are probably the happiest.
MOLLY
I wonder, too, on the support side of the equation, how even having the human-to-human touch of lactation support has a role. Having a person you know by your side. I think that's a big part of doula care and why you see positive outcomes – you have your person, this extra layer of social support.
ANDREA
Having the data point to validate what you just said would be interesting to study. For SimpliFed, we have a virtual providers and the question is usually, “how do you do lactation support virtually?” Well, first off, there is a lot you can do on the phone. The thing about elbow-to-elbow care is that when someone’s placing the baby on your breast that works for like 10 seconds, but then when the lactation consultant leaves, you still haven't built that muscle memory.
“I would be really interested to see emotional and mental health outcomes for combo feeding compared to those who are totally breastfeeding or totally fully formula feeding. My hypothesis is that the halfsies are probably the happiest.”
I've had eight appointments with SimpliFed. They each last an hour. I’m getting educated. It’s preventive care in so many ways.
I am now two days away from reaching the AAP six months exclusive breastfeeding goal, which I didn't actually have as a goal when I started! But, yeah, I am reaching it. Because I got hooked up with support. And I feel great about it because I got nowhere near that with my other babies.
MOLLY
I find it so fascinating that, here you are, mom of three, founder of a company that provides baby feeding support, and you are like “six months is such a huge accomplishment!”
I think that just speaks, again, to the importance of support. Like you said, you have the financial stability to do all this, you live in like the land of lactation support AND you still really benefited from having this full extra layer of individualized support.
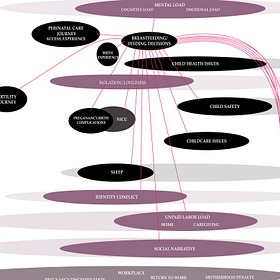
For the stressor map – that support could alleviate the stressor connections to the social narrative. It also plays into isolation, loneliness. It plays into any additional access to care issues from the prenatal care experience, with those acting like scar tissue in a way that affects perception of the stress related to feeding.
Is there anything else on the stress map that is calling to you and worth a deeper exploration? In your personal or professional experience?
ANDREA
Breastfeeding and baby feeding are definitely connected to all of this.
There is isolation and loneliness; we see this a lot with our military families. They don't have family around right to help and maybe don't have friends that they feel comfortable with. So they are just so isolated and just toiling by themselves.
Baby feeding is so connected to childcare issues, if you think about it. When I'm sitting there breastfeeding, I can't run after our toddler. When you're breastfeeding all the time, on demand, unplanned, it can be extra tricky if you don't have childcare. It relates, of course, to child safety. It relates to the tremendous unpaid labor load – there are no days off, no nights off. And that makes it obviously deeply connected to sleep. Any birth complication with you or the baby; like if you have a C section, breastfeeding is a lot harder.
It's all connected.
We especially see this interconnection a lot with our patients who went through fertility treatment. They want to breastfeed and are often a bit ride or die about it because they think, “I went through all this. I want to give my baby the best”. It’s important to remember that if you are not well, that's not giving your baby the best.
Yeah, it's connected to all the things.
MOLLY
I actually did not have the breastfeeding stressor node connected to the fertility journey before now. I had been thinking “is this actually connected?” and then you make this important point that going through fertility treatment elevates the preciousness of doing everything right. Not to mention adding in pregnancy and birth complications.
It was already connected to the NICU stress because the NICU feels like a very specific case. I mean, what do you see working with like C-section patients and NICU parents?
ANDREA
It's very different. The first two weeks are very different. For c-sections, you have this wound. A lot of breastfeeding is about holding but it's really painful to be holding a baby right there. And obviously, it's deeply connected to the NICU too, especially if your baby has low birth weight.
A lot of the research literature is ambiguous and gray about the connection between baby feeding and baby’s health. But the one area of research where it is crystal clear is that any breast milk is better for NICU babies. The order is: breast milk then donor milk. I am not in the breast is best camp, which a lot of people find surprising; I am very much in the whatever works for you camp – what works for your mental and physical health. But in these specific cases, for example, I was on the phone with a neonatologist who studied this and she said, “Yeah, that's the cool thing about breast milk. It's tailored to your baby's needs. And so donor milk is awesome, but we just don't see the same outcomes with donor milk compared to your own human milk.”
MOLLY
How is that reflected in support? Or how has that fallen short, in terms of aligning the pressure on the lactating parent to breastfeed versus pressure to make sure resources are available in the NICU?
ANDREA
What we see with our NICU moms, because the data [on the benefits of breast milk] is so clear, is that they get crazy pressure. Shamed when they're already going through a lot. One of the things that we're working on, because it's very nuanced, is scripting language that's still providing evidence to patients, while not being anti formula. It's extremely hard.
Shame is just embedded in the words, sometimes. I had a physician once say to me “Well, if you had gotten support with breastfeeding, you would have breastfed for longer.” And I fucking hated her. I was like, “that’s the meanest thing you could say to me”. And here I am saying that!
“What we see with our NICU moms, because the data [on benefits of breast milk] is so clear, is that they get crazy pressure. Shamed when they're already going through a lot.”
This is the tough part – providing evidence when evidence is actually triggering. So, what I would like to see is scripted language that is still evidence-based, without being judgmental.
MOLLY
So maybe we should be using the data on the importance of the parent’s breast milk to create more support and implement better support measures to help individuals overcome challenges; rather than taking that evidence and going straight to the lactating parent and saying: “You need to at all cost because breast is best.”
ANDREA
The key thing here is saying: “Here are your options. Let’s go through options and based on what’s resonating with you, let’s chat. Ok, you want to chat more about it? You want to talk about what this commonly looks like?”
Then this is what we are hypothesizing – by being inclusive with feeding choices, you will see higher breastfeeding rates.
For me – my goal was not six months exclusive breast milk feeding. I was happy to combo feed. Combo feed away! For me, we got a shit ton of support. And here I am about to hit the six month mark because I felt comfortable and everyone agreed with the things I needed.
At one point I said “I think I'm gonna start using formula because I'm about to go on this work trip…” and [my lactation support team] was like, “you can, you absolutely can, but just so you know, you don’t need to. Your supply is good.” That’s a good way to play it – if you want to do this, awesome; if you want to do that, great.
That’s the type of scripting that I think needs to be proven or shown or studied.
MOLLY
Along with making sure that the support and the structures for that support are in place.
ANDREA
Nailed it.
Coming up next – Let’s decode it all!
In a follow-up to the follow-up, we tackle the stressor map to explore additional factors that contribute to the perception of stress at this node and look for solutions at all of those connection points.
Reducing the stress of modern mammalian motherhood
When it comes to breastfeeding and baby feeding decisions, the stress is layered, the connections are personal and, somehow, also universal.
Quick note about subscriptions: The Maternal Stress Project is an educational and idea-spreading initiative and I want it to be available to all. You can subscribe for free and get all posts delivered right to your inbox. However, if you feel compelled to bump up to a paid subscription, your generous support will facilitate the growth of this project… and be much appreciated!
Sharing and spreading the word is equally valuable and appreciated!